Organ Transplantations Timeline 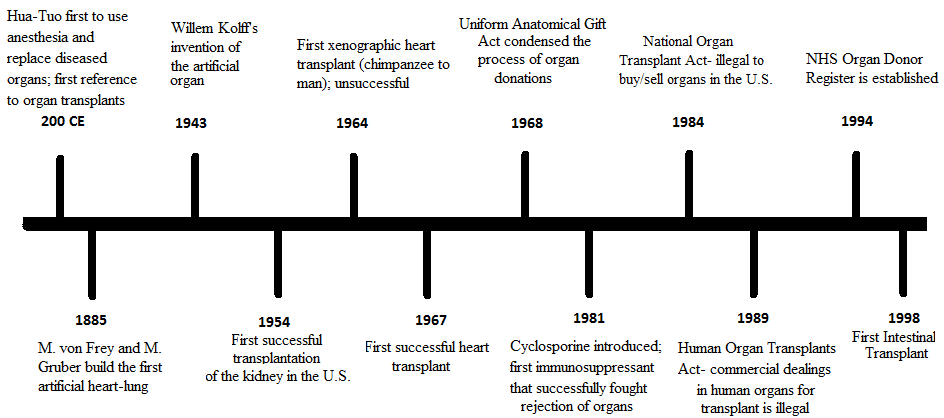 |
||||
When, where and why was this developed? Organ transplantations were noted to have developed around 200 CE by a Chinese doctor by the name of Hua-Tuo. However, the first successful transplantation was of the heart and had not taken place until 1954. In 1885, M. von Frey and M. Gruber built the first synthetic organ to study. The man credited to have invented the first working artificial kidney was Doctor Willem Kolff who was born the Netherlands but moved to the United States. His invention was created in 1943. Of the fifteen people his invention was tried on, only one survived.[4] Though the numbers may be small, a new breakthrough occurred. Artificial organs were made as an alternative to risky allotransplantations. Because organ recipients and the number of patients on the donor waiting list continued to increase, while the number of donor organs did not, scientists were looking to create synthetic organs as a substitute to a physical organ.

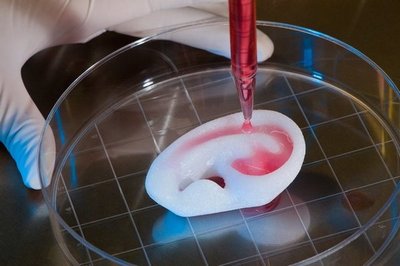
Regenerative Medicine + Organ Transplants: When combining regenerative medicine with organ transplantations, the desired outcome is to create living and functional tissues to replace or repair organ or tissue functions. This field has the potential to solve problems of organ shortage and harms from immunosuppression. The cells in a regenerated organ would match the cells from the patient in which they were derived from. Regenerative medicine combined with organ transplantations has received remarkable results which has caught the interest of the transplants community.[7] In an example story of the successes of regenerative medicine, a boy received a replaced trachea with his own stem cells. The process started with a donor trachea taken in and stripped off of its cells. The boy's stem cells were infused into the trachea and it was placed surgically into the boy. There was no risk of rejection because the boy's own cells were used in the process.[8]
The Future: Scientists in the field of regenerative medicine expect to achieve these several things to occur in the near future: -New methods that make it easier to regenerate the skin, bone, bladder, trachea, heart and heart valve - Restoration of functions in complex tissue -pursuing the goal of regenerating neo-organs.[10] -ensuring that these treatments are both safe, effective, and approved by the FDA -"confronting major challenges such as identifying cell sources and clinically relevant cell numbers, the integration of new cells into existing tissue matrices, and the achievement of functional properties of tissue equivalents using an expanded repertoire of biomaterials" ("Future in Regenerative Medicine"). [11] |

How does this technology work? Artificial man-made organs are aimed to replicate the function and appearance of a natural organ. The artificial heart was made by Robert Jarvik in the 1950's. He worked on a team along with Willem Kolff and his invention was called the Jarvik-7. The Jarvik-7 was made from dacron polyester, plastic, and aluminum and had an internal power system that regulated the pump through a system of compressed air hoses. The patient who first tried the Jarvik-7 only survived for 112 days.[5] Since then Dr. Robert Jarvik has work on a new, improved thumb-sized artificial heart called the Jarvik-2000. Unlike a natural heart, the Jarvik-2000 does not beat, but instead uses a rotor to propel blood from the left ventricle into the aorta. It is also electrically powered. The difference between the Jarvik-2000 and the Jarvik-7 is that the Jarvik 2000 restores a weakened heart to have normal blood flow. [6]

Major Challenges: Many challenges face advancement in the usage of regenerative medicine more often. Some include factors in stem cells which limit their usefulness in this science. These issues include problems with accessibility, restricted variations, and poor growth of the cells. Furthermore, there is roughly only one stem cell for 100,000 bone marrow cells. Some cells used in regenerative medicine can only divide a finite number of times, depending on the age of the donor, which limits the supply. The use of embryonic stem cells because of their relentless capacity to multiply is considered to have significant possibilities in regenerative medicine. However, ethical issues have become a problem and lessen the potential of their usage. Research which has developed into this new technology was very critical and challenging. This tough technology needs to be fully developed and harmless before using it on a patient. Scientists are working to better develop so that they can be secure with using regenerative medicine on patients.[9]
|
|||